Michael Garron Hospital
Michael Garron Hospital, a busy community Hospital situated off the Danforth in the heart of Toronto, is seeking four outpatient psychiatrists. The positions involve backing up a team of non-medical therapists for crisis intervention, as well as developing outpatient clinics for major psychiatric disorders There is an opportunity to serve the community while growing personal psychiatric interests. The position is financially competitive, and offers an opportunity to have senior colleagues provide mentorship in the transition. The clinical work is diverse and interesting. The hospital location offers an opportunity to live and work in relatively central Toronto.

The goal of the Department of Psychiatry and the Mental Health Service is to optimize patient outcomes while working to increase the capacity of community-based clinicians and agencies, to treat psychiatric outpatients.
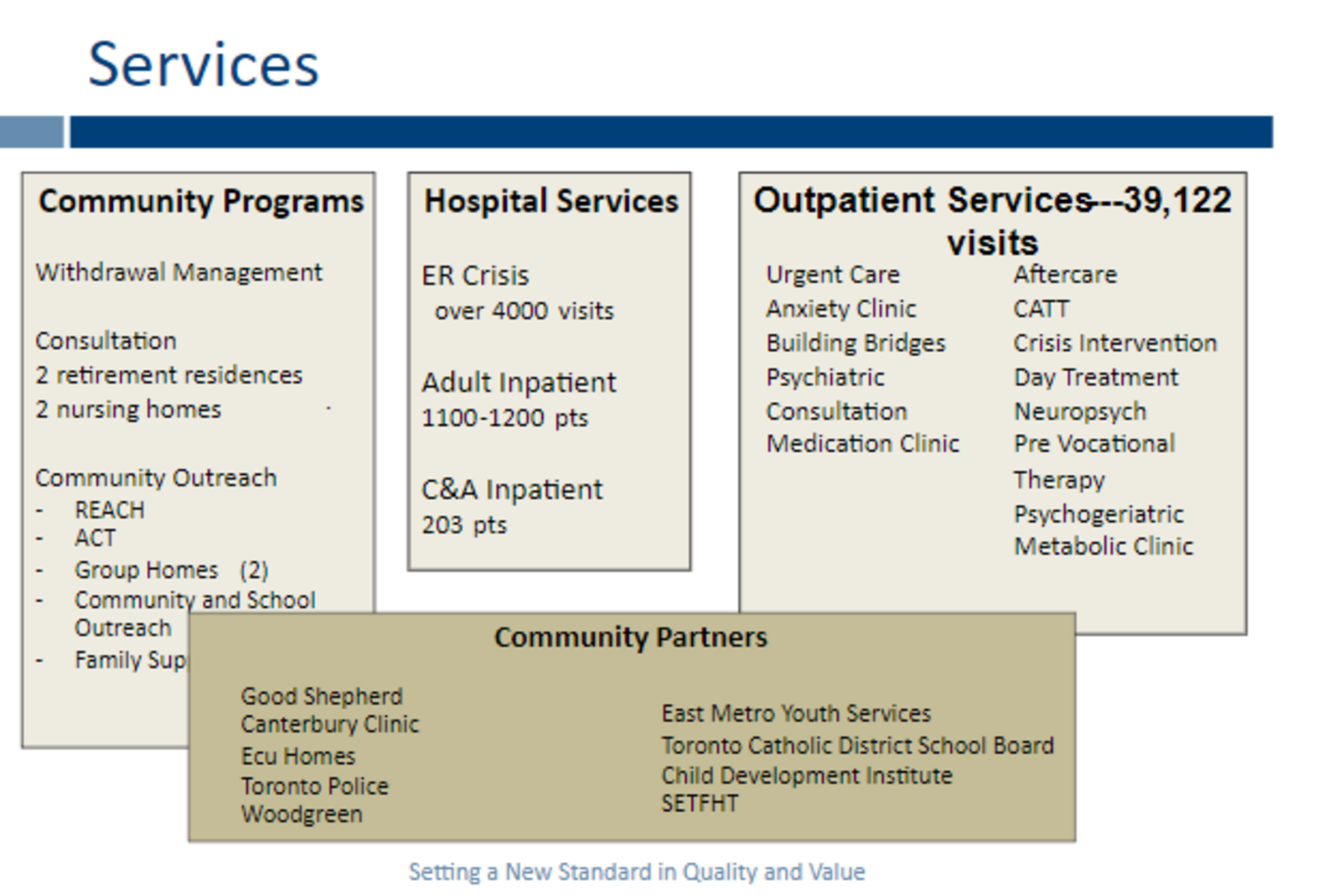
At Michael Garron Hospital we have a broad array of services.
As part of a hospital wide initiative, we have been involved with the creation of an Ontario Health Team to achieve greater integration of hospital and community agency services to improve care for our community with regard to psychiatric and substance related services. In the field of addictions, we are collaborating to provide coordinated and rapid access to care with community and hospital partners.
The hospital service and department have been involved in creating the East Toronto Health Partners Adult Mental Health Working Group. The purpose is to lead strategic planning, integration and coordinated service planning, organization and delivery across all sectors involved in adult mental health in East Toronto with the goal to improve care for adults accessing mental health services. This involves setting strategic priorities and develop operational objectives, policies, practices and activities to facilitate integration and coordination of ETHP adult mental health services, and to promote collaboration between organizations, staff, physicians (including primary care) and the greater community toward meeting strategic priorities of ETHP in adult mental health, and to collaborate with the ETHP Digital Committee to develop digital approaches to care navigation, delivery and information sharing to support integration across ETHP, and to harmonize client, caregiver and provider education and support programs, policies and practices across the ETHP adult mental health providers.
We have consolidated our transitional youth program, which is a three month clinical navigation for 16 to 29 year olds experiencing barriers or struggling to engage in services within the mental health system, providing brief clinical support and system navigation to hospital community clinics, and support with transition to adult mental health services. In the first two years of the program we received 500 referrals, of which 80% are successfully engaged in the program with two or more visits; with almost 50% discharged as connected to another service, 26% of discharged did not want or need a connection to another support, and 39% less likely to have problems associated with accessing services and supports. Also there was a substantial decrease in emergency room visits for those involved with the transitional youth program
The Michael Garron Hospital Paediatric and Child and Adolescent Mental Health Services are exploring a collaboration with the Extensive Needs Service, a partnership between Holland Bloorview, the Children's Hospital of Eastern Ontario (CHEO), and McMaster Children’s Hospital. This service is aimed at addressing the particular needs of children up to age 18, whose complex needs have not been met by existing services and who are experiencing frequent emergency visits or referrals to urgent and crisis services. Presentations include challenging or interfering behaviour of at least 12 months duration, safety concerns, impaired functioning, and complex caregiver needs, despite the involvement of three or more providers. These children and youth live with co-occurring neuro-developmental conditions or acquired brain injury, mental health conditions, and chronic physical health conditions. The collaboration will provide funding for local, intensive and individualized services for these children, youth and families, to include mental health assessment and treatment, psychopharmacology, specialized and intensive behavioural intervention, parent support, allied health treatment such as occupational therapy and speech and language pathology, respite, and transition support to school, community services and adult services. We are excited to explore the potential for this important collaboration to support the children and families within our local communities.
With regard to quality improvements, and we have been interested in certain metrics. For example, falls on the inpatient unit for the last 13 years were between 30 to 66 falls per year. In the last year since we implemented adjustments, including bed alarms wireless nurse calls, and special falls risk prevention beds, the falls decreased to seven. Similarly, we are pleased that the results when we focused on workplace violence prevention. Through different interventions, workplace violence has fallen from 56 incidents five years ago to three incidents last year. We have focused on following up emergency visits within 30 days of discharge, and have seen a yearly decrease in the percentage of patients who went to emergency within 30 days of being discharged. Also we have been focusing on decreasing our length of stay, and we have been successful in this regard despite some outliers.
Our Goals:
- improve access and optimize the quality of psychiatric care
- improve capacity of community providers to treat individuals in the community
- improve continuing education of our staff and community providers
- create new Out Patient programs to serve the different needs of the different services in the hospital and the community (e.g. Oncology, Maternal newborn)
- explore on-line services/innovations to improve the patient’s experience
- identify additional ways to obtain feedback and incorporate patient voice into planning
Thus, by emphasizing education, innovation, collaboration and integration, and responsivity, we strive to optimize clinical care of those challenged with mental health issues both acute and chronic, and increase the capacity of community-based clinicians and agencies, to engage and treat patients more effectively.
Michael Rosenbluth MD FRCPC
Chief, Department of Psychiatry,
Michael Garron Hospital/Toronto East Health Network
Associate Professor, University of Toronto
